I was part of a special emphasis study section last week titled – “Circadian Patterns of Gene Expression Associated with Disease” for RFA-HL-20-016. The RFA was sponsored by NHLBI and NIDA, so most of the proposals revolved around priorities of these two ICs. Program Officer mentioned that it took 3 years to secure funding for this RFA. The underlying message was that circadian work is difficult to fund. We in the circadian field have always known that our fundamental work on circadian biology is difficult to fund. This is mainly because circadian research has always been an orphan. Although it is now recognized as a contributor to everything from metabolism to Alzheimer’s and beyond, traditionally there has been a lack of direct diseases associated with circadian disruptions. For instance, mutations in core clock genes are not associated with diseases that affect large numbers of people. As John Hogenesch likes to point out most knock outs of core circadian genes are viable. Until a few years ago, the connection between circadian rhythms and metabolism, heart disease, AD was not established. Therefore, circadian biologists have always had to struggle to shape their research to fit a particular IC at NIH. In essence, circadian rhythms effect so many biological processes that it is an orphan.
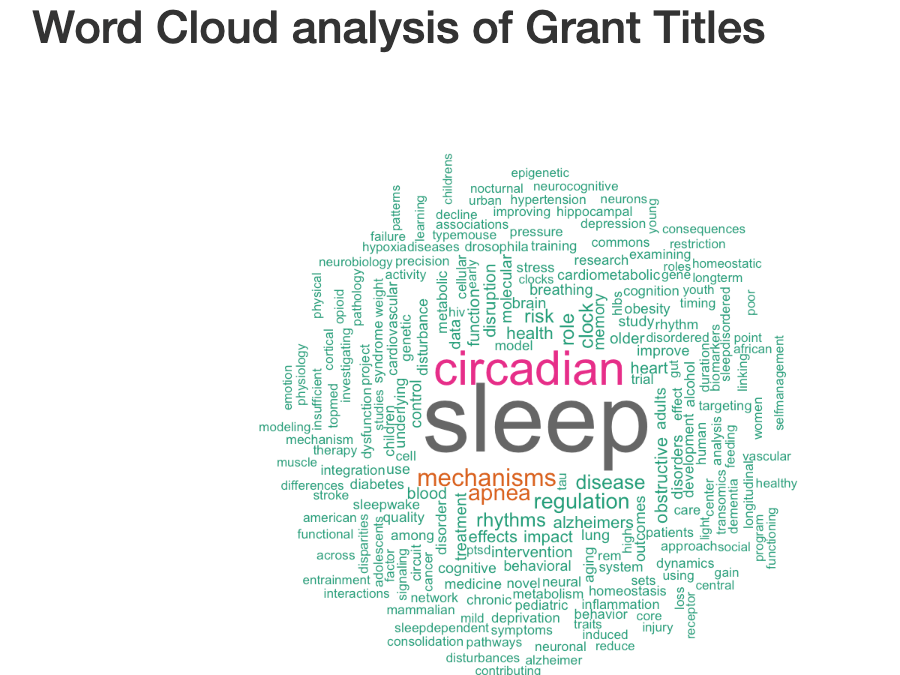
I did an analysis of who is funding circadian work at NIH. The data is downloaded from NIH Reporter and looks at the term “circadian” or “sleep” in the title. The primary data is here. The analysis code is here. These are “active projects”.
How many projects are funded for Sleep and Circadian?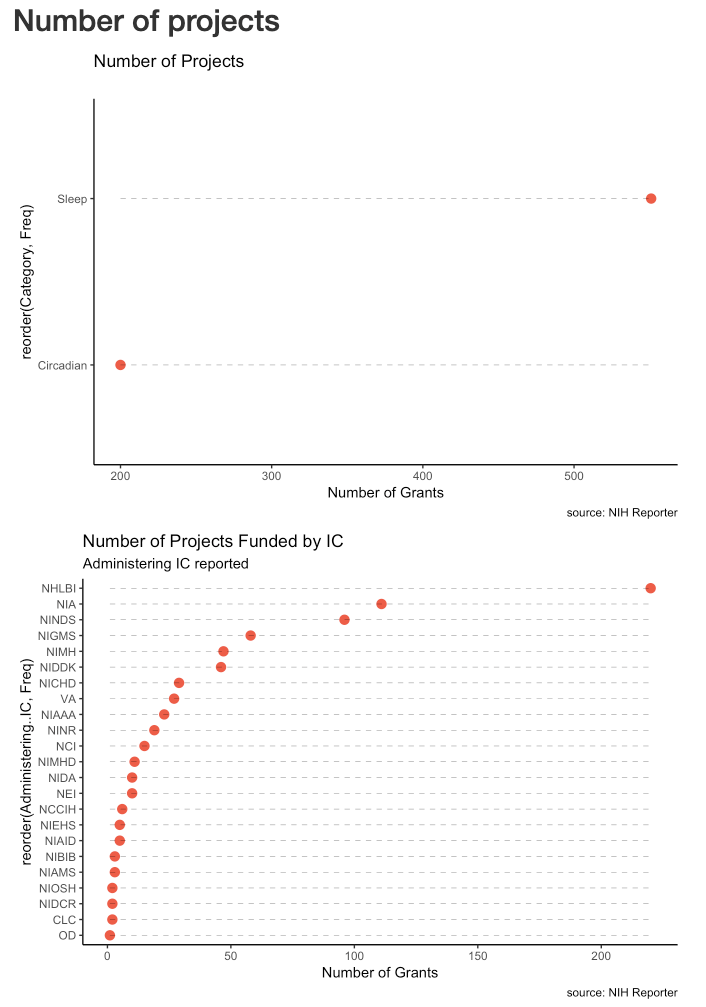
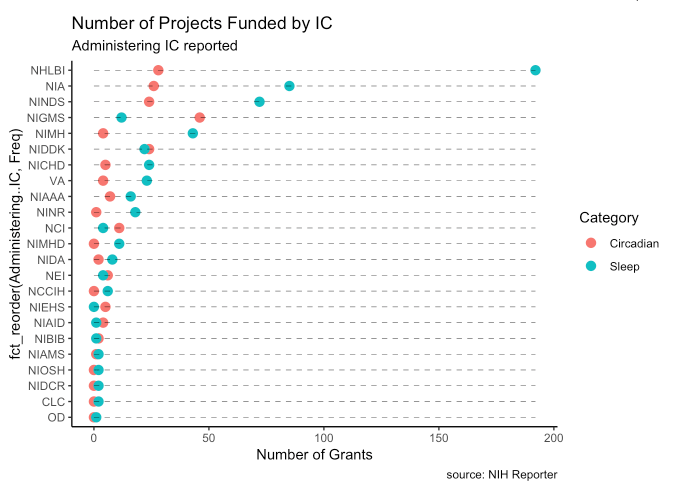
There are roughly 3 times as many sleep projects as circadian. NHLBI, NIA, NINDS, NIGMS, NIMH, NIDDK sponsor the largest number of projects.
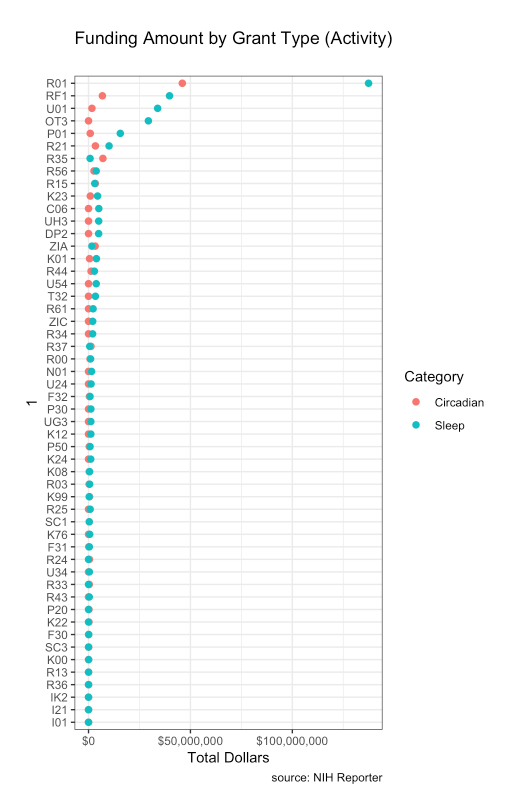
How much money is spent for circadian or sleep research?
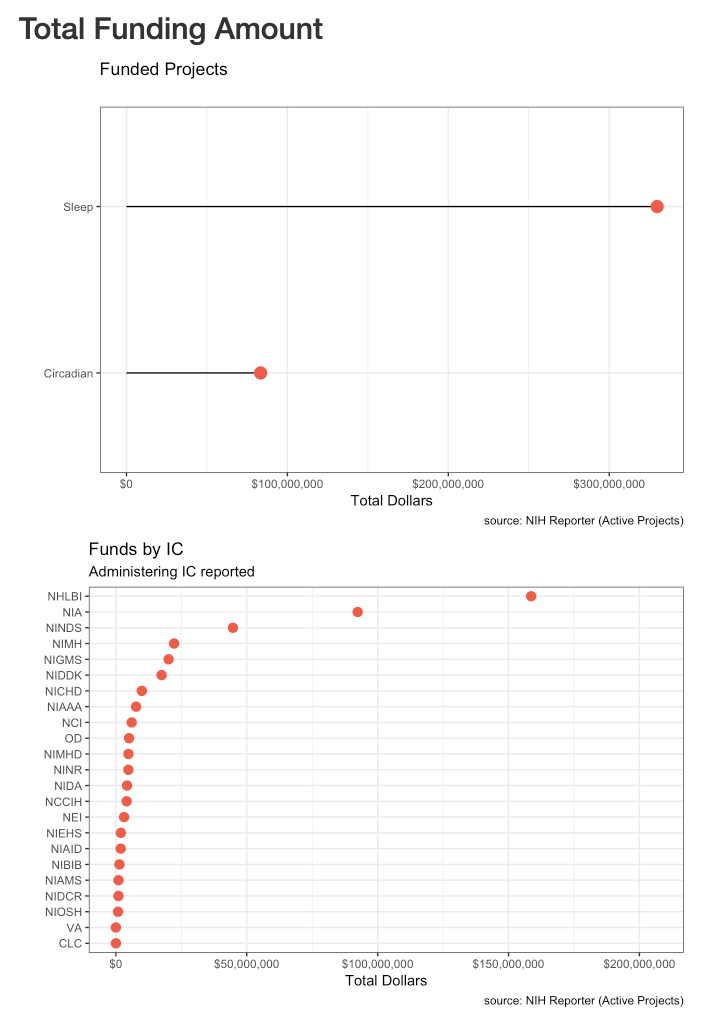
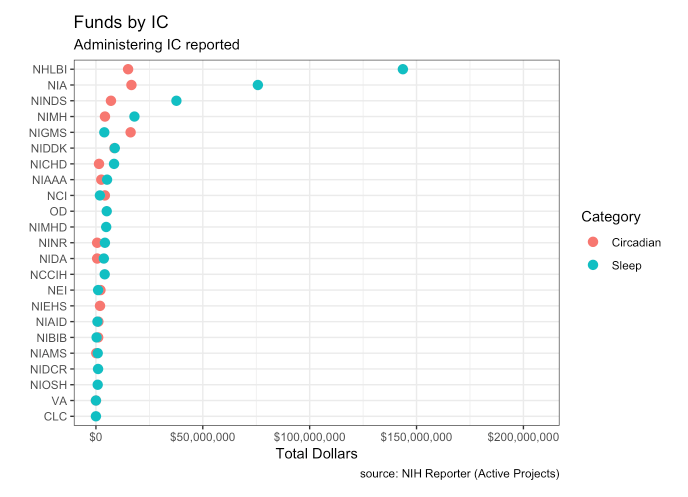 NIH actively roughly $400 million to study sleep and circadian rhythms. The dollar amounts reflect the number of projects. NHLBI spends the most with a little over $150,000,000 for circadian/sleep projects currently. Most agencies spend far more on sleep research than circadian (NIGMS is an exception).
NIH actively roughly $400 million to study sleep and circadian rhythms. The dollar amounts reflect the number of projects. NHLBI spends the most with a little over $150,000,000 for circadian/sleep projects currently. Most agencies spend far more on sleep research than circadian (NIGMS is an exception).
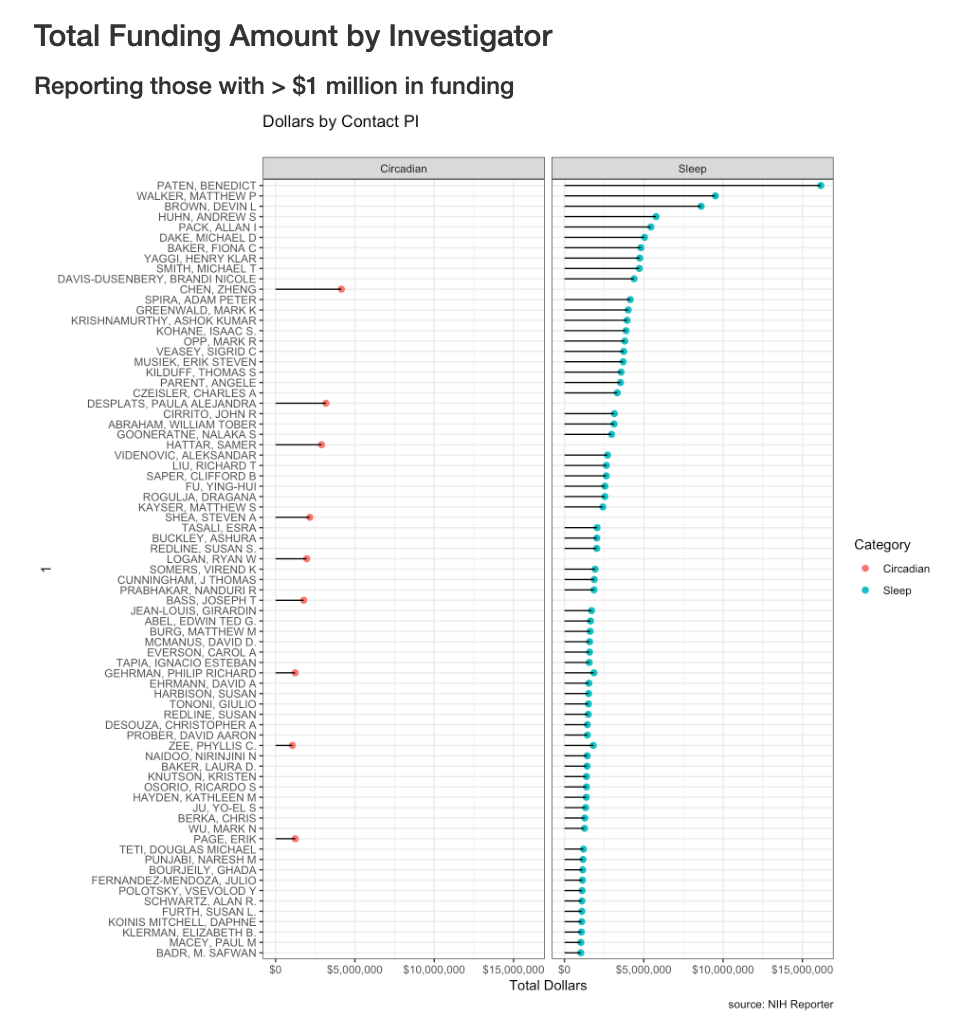
Top investigators who receive the most funding.
This should be interpreted with caution. I’m using the contact PI. Many grants are consortium agreements and multiple PIs and the dollar amount going to contact PI can vary.
 Types of grants
Types of grants
Not surprisingly, most of the dollars are spent in R01s.
Conclusions
Circadian and sleep are linked yet independent processes. In terms of importance, as a circadian biologist, I’m biased. Circadian system has molecular mechanisms and very useful tools to elegantly dissect mechanisms. Sleep is still amorphous in terms of mechanism and even function. This may be a reason to spend more to study sleep biology. However, I’m surprised that NIMH, NIDA, NCI, NEI do not have a larger portfolio of circadian projects. This may be because more diseases have traditionally been associated with sleep disruption than circadian dysfunction. For instance, Disease Ontology, lists 14 sleep terms, but no circadian terms. DSM-V lists “Circadian Rhythm Sleep-Wake Disorders” as one combined disorder. I believe this will change as the impact of circadian regulation becomes more apparent in metabolic disorders, heart disease, and psychiatric illnesses.I don’t want to make the argument that sleep funding should be transferred to circadian, but rather that more funding be directed towards circadian to balance the two fields. The RFA that NHLBI and NIDA sponsored last week, is a good example of how this can be done.